How many lives does a doctor save? (Part 1)
An invocation to I-em-hetep, the Egyptian deity of medicine. Oil painting by Ernest Board. Source: Wellcome Library, London.
This is Part 1 of an updated version of a classic three-part series of 80,000 Hours blog posts. You can also read updated versions of Part 2 and Part 3. You can still read the original version of the series published in 2012.
Doctors have a reputation as do-gooders. So when I was a 17-year-old kid wanting to make a difference, it seemed like a natural career path. I wrote this on my medical school application:
I want to study medicine because of a desire I have to help others, and so the chance of spending a career doing something worthwhile I can’t resist. Of course, Doctors [sic] don’t have a monopoly on altruism, but I believe the attributes I have lend themselves best to medicine, as opposed to all the other work I could do instead.
They still let me in.
When I show this to others in medicine, I get a mix of laughs and groans of recognition. Most of them wrote something similar. The impression I get from senior doctors who have to read this stuff is they see it a bit like a toddler zooming around on their new tricycle: a mostly endearing (if occasionally annoying) work in progress. Season them enough with the blood, sweat, and tears of clinical practice, and they’ll generally turn out as wiser, perhaps more cantankerous, but ultimately humane doctors.
Yet more important than me being earnest — and even me being trite — was that I was wrong. Medicine was not my best option for helping others when compared to all the other work I could do instead. And I think that is not just true for me in particular, but for many able, altruistically minded people considering a medical career.
This series of posts will explain why.
- Part 1 covers the impact of medicine on human health and disease. Upshot: medicine as a whole, at least as practiced in most clinical settings, has been only a minor player in the dramatic improvements in human health over the last couple of centuries (relative to things like nutrition, safer jobs, and general scientific knowledge), so one should expect the impact of providing more of it now by working as a doctor to be fairly modest. Unlike what you see in the medical dramas where the protagonists are saving lives every episode, it is more like saving a couple of lives every year. This is better than the direct impact of most jobs and might still make a compelling case for pursuing this career path if not for other considerations covered in parts 2 and 3.
- Part 2 takes a closer look at the impact of you working as a doctor in particular. Upshot: thanks to issues like diminishing marginal returns and replaceability, adding another doctor (you) to a place like the UK would be expected to have an even more modest impact than that of medical care in general. Instead of saving a couple of lives every year, it is more like saving a few lives per career.
- Part 3 will look at possible ways medics can have an outsized impact, such as earning to give or working abroad in lower-income countries.
Is medicine a determinant of health?
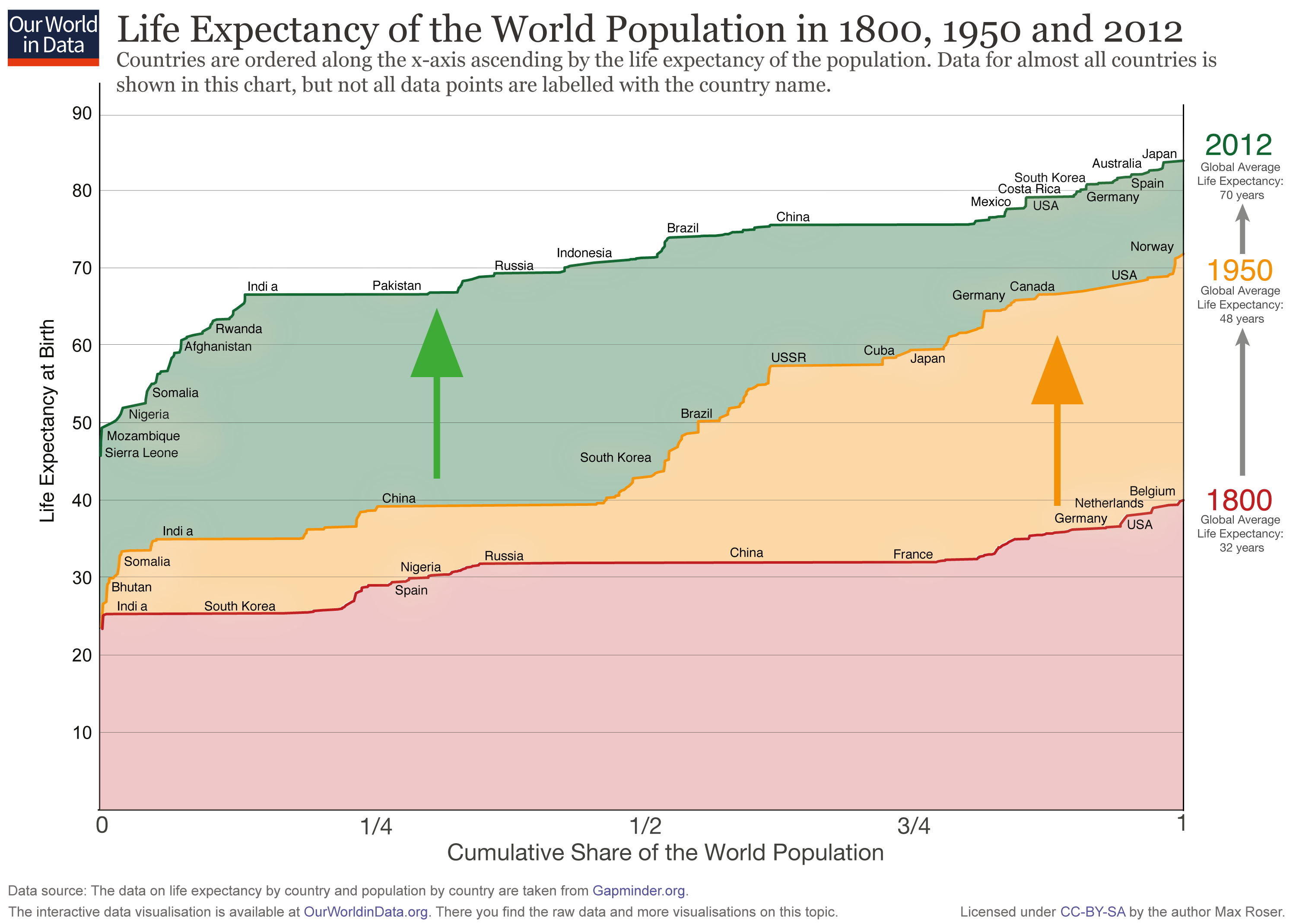
On average, it’s clear that humans live much longer and healthier lives now than we did a century or two ago. Exactly why this has happened — and how much credit medicine can claim for us being healthier — is much more uncertain.
UK1 life expectancy doubled from 40-ish in the 1800s to 80-ish now. The largest contributor was a reduction in infant and childhood mortality. For example, in the UK, around 15% of those born in 1900 died before their first birthday — now it is ~0.4%. But survival has improved in every age bracket.
This trend is basically universal. There remains a lot of global inequality in life expectancy, and the upward trend has disruptions, most recently due to COVID-19. But wherever they are born, children today can expect to live (at least) twice as long than those born in the 1800s.
One story explaining this trend attributes it to advances in medical care. Nineteenth century medicine was much more primitive than 21st century medicine: antibiotics, vaccines, chemotherapy, defibrillators, surgery, and (effective) drugs basically did not exist. So perhaps we live longer thanks to modern medicine fending off the scythe of death.
Although this is part of the picture, it is probably a small one. The dramatic improvements in health over the last two centuries are attributed less to medical care and much more to the social determinants of health.
In essence, living standards have improved, humankind got dramatically richer, and we’re better informed than we used to be. These key changes enabled us to do a bunch of things to prevent illness in the first place. Some examples (among many):
- A population learning the basics of public health — like germ theory or “smoking kills” — means individuals can better avoid disease. If rich enough, they can also afford public works like sanitation systems, curbs on air pollution, and fortifying common foods with micronutrients.
- Richer populations tend to have a lower proportion working in more dangerous industries. More people work in services like hospitality or finance, while fewer people work in agriculture and manufacturing. At the same time, dangerous occupations and transportation can be made safer.
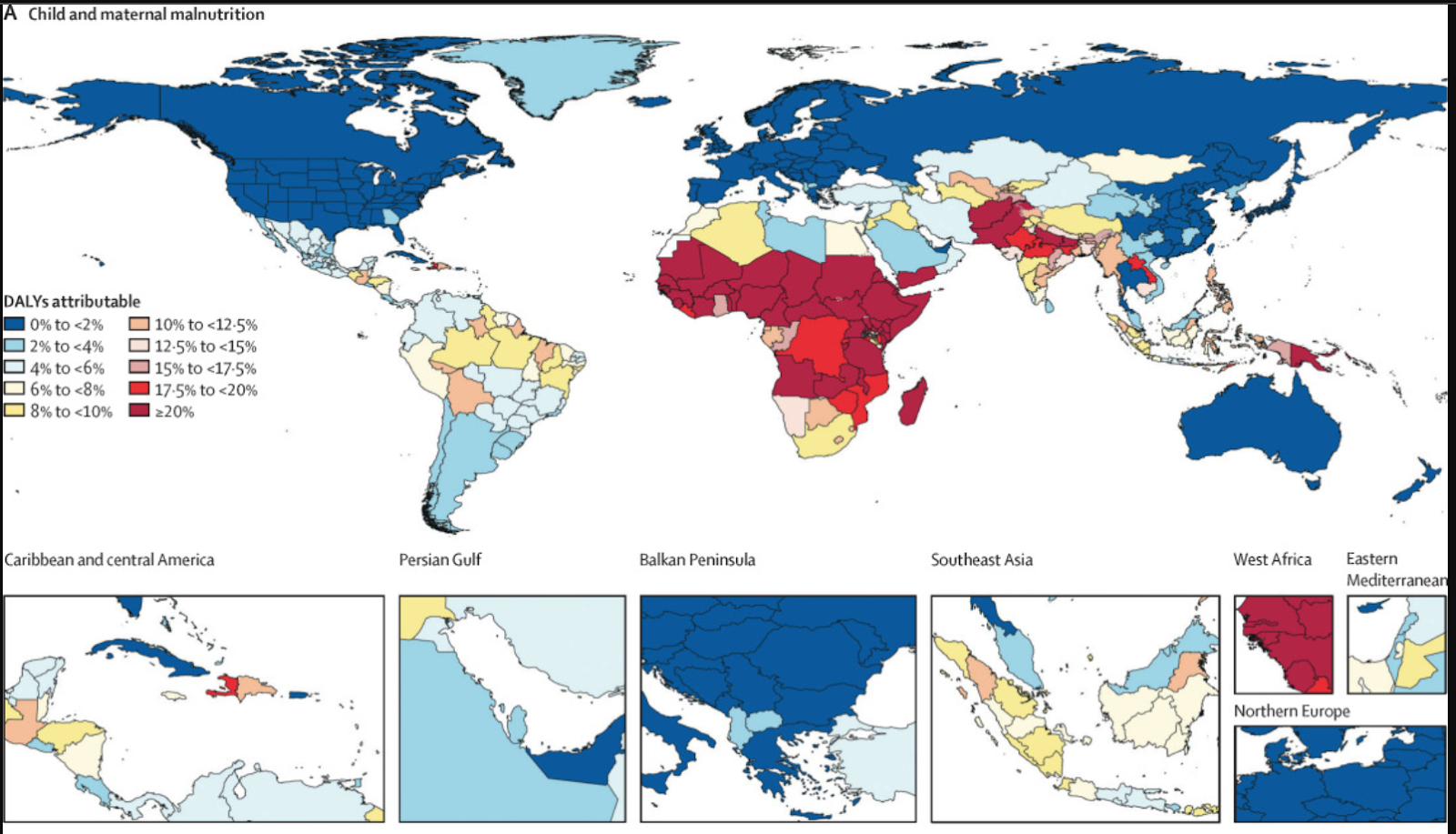
- Richer populations can feed their children enough, setting them up for healthier lives as adults. Height used to be an excellent indicator of wealth because poverty led to childhood malnutrition and stunted growth. Maternal and infant malnutrition remains among the biggest risk factors for ill health worldwide, but it is largely absent in high-income countries.2
Evidence from a few different sources indicates that it is mostly these social determinants rather than medicine that do the heavy lifting for health and longevity:
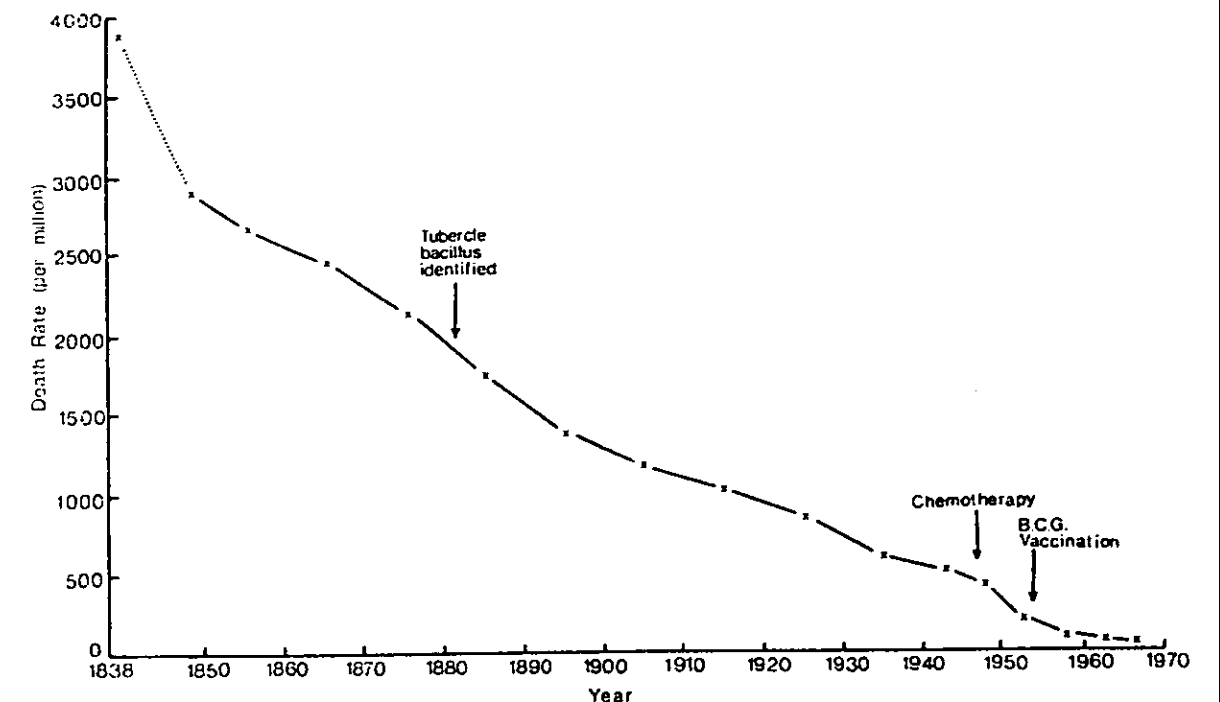
- Mortality trends show that death rates often started decreasing prior to many major healthcare discoveries. The canonical example is tuberculosis: mortality fell ~30% before the bacterium was identified, ~80% before effective drug therapy, and ~90% before vaccination.3

- Good ‘per capita’ healthcare spending figures are trickier to find,4 but available evidence shows that the explosion in health spending happened after the skyrocketing of life expectancy. Here are some suggestive figures for the US:
Life expectancy Health spending per person (inflation adjusted)5 1890 45 Uncertain, but surely <$151 1960 70 $151 2020 77 $12,600 - There have been a couple of studies randomising people to receive more or less access to healthcare in the US. Although interpreting these studies is tricky, it is fair to say better healthcare access resulted in very minor health gains.5
- Observational data of intra-national inequality in health outcomes by occupational class, income, education (etc.) are also consistent with the theory that social determinants have driven health improvements.
- If you compare different countries by how healthy they are (whether by life expectancy, disability-adjusted or quality-adjusted life expectancy, or aggregate measures of ill health), the best predictors are measures of wealth (e.g. GDP per capita) or education (e.g. years of schooling). Controlling for these factors, measures of healthcare (e.g. doctors per capita, health spending per capita) have negligible impact (much more later).
Ironically, the picture of the man holding off the scythe of death above may be — inadvertently — right after all. Although the man is meant to represent medicine (the frieze is on the side of a hospital), he is holding the wrong symbol. The rod of Asclepius, god of medicine, only has a single serpent and no wings on the top. Instead, the man is holding a caduceus (two serpents, wings), the staff of Hermes. Although the caduceus is widely used as a symbol of medicine, this practice originated in the US in the 20th century and is generally deemed an anachronistic confusion.
But if you are going to fend off the scythe of death, maybe the caduceus is the better stick for the job. Hermes is not the god of medicine; he is the god of trade and commerce, and the caduceus has sometimes connoted wisdom and knowledge. So perhaps it is a better stand-in for what has doubled lifespan over the last two centuries — our growing wealth and wisdom — and Hermes has done better than Asclepius so far.
Medical care (and medical careers) in context
Although health is mostly a matter of social determinants versus medical interventions, the latter still matter. Some relevant nuances:
- For some diseases, it is obvious that medical interventions are the decisive factor in reducing mortality. Consider type-1 (insulin dependent) diabetes: prior to insulin therapy, this early-onset disease was inevitably fatal within a couple of years. Today, those with type-1 diabetes still have ~10-year shorter life expectancy than those without, but essentially all the credit for changing this disease from ‘childhood death sentence’ to ‘reliably surviving to adulthood and often old age’ goes to medicine. There’s not much of a social determinant story to tell for improved outcomes from this disease — indeed, its incidence has been steadily increasing.
- Although most (either by count or prevalence) conditions have mortality graphs that look like tuberculosis, some — such as polio and smallpox — do show dramatic declines following vaccine deployment.
- Although cardiovascular disease and cancer (the main causes of death in richer countries) have a variety of lifestyle risk factors, medicine has made steady progress in both improving treatment and using drugs to reduce risk. So the balance of expert opinion tends to attribute a significant part of the steady incremental improvements in health in wealthy countries over the last 50 years to these medical interventions.6
I think the overall picture is shown by the Global Burden of Disease project. Communicable, maternal, neonatal, and nutritional diseases are principally diseases of deprivation, where most of the battle is won through improving the social determinants of health. Winning this battle, as countries like the UK (mostly) did between ~1800–1950, and many others have done since, gets you from a life expectancy of ~30 to a life expectancy of ~70. Climbing from there is mostly a steady slog against non-communicable disease.
In this regime, medicine has two important roles. First, the social determinants greatly reduce individual risk and the population burden of disease in youth and adulthood, but eliminate neither — medicine can help pick up the pieces for those who get unlucky. Even a hypothetical ideal public health population of affluent, well-educated, never-smoked, BMI 22, teetotaler triathletes will have some who suffer life-threatening accidents, others who develop rare conditions like type-1 diabetes or childhood cancers, and even some who have high blood pressure and cholesterol. Real populations like the UK fall well short of this, even if they are much closer to the ideal than they are to the prevalent poverty of the 1800s.
In old age, everyone’s luck runs out eventually. The second role of medicine is fighting a rearguard action against the progressive bodily breakdown of ageing. Its successes here are less dramatic and more incremental. Medical science has few solutions to many of the diseases of old age. Treatment is complicated by comorbidity and multiple organ systems developing varying degrees of failure (e.g. life-saving surgery or chemotherapy is much more treacherous when the patient’s heart, kidneys, and liver are not what they once were).
The steady development of multiple life-threatening diseases means even if a doctor can save their elderly patient’s life, they will likely succumb to another not too long thereafter; curing an 80-year-old’s cancer is unlikely to give them a new 30-year ‘lease on life’ like it might for a 20-year-old.7
So the answer to “What has modern medicine ever done for us?” is, relatively speaking, not all that much. Although some of us will have our lives or limbs saved by medical care, for most of us the impact is smaller: potentially making some chronic diseases a little better and making our old age somewhat longer.8 So, perhaps joining the medical profession is worthwhile, but maybe not as great in terms of humanitarian impact as tropes would have you believe.
An initial number for how much good doctors do
I still haven’t answered the question of how many lives a doctor saves: ‘less than the industrial revolution’ doesn’t narrow it down much — everyone living a bit longer, and no one dying of smallpox, still matters a lot. And that medicine’s aggregate impact on the human condition is relatively modest versus other factors could still mean one’s contribution as a doctor is great in absolute terms.
It is tricky to work out the precise fraction of health medicine can take credit for, but here’s one attempt from researchers John Bunker, Howard Frazier, and Frederick Mosteller. In essence, they look at the most important medical interventions (gathering enough to cover most of the benefits from medical care), get quantified estimates of their efficacy from trial data, and then estimate the aggregate benefit from how commonly these interventions are made.
They estimate approximately five of the 30-year gain in life expectancy in their population was owed to medical intervention and another five years ‘relieved’ from poorer health.
These estimates are rough,9 but we can use them to generate an even rougher back-of-the-envelope figure. We’ll first translate this estimate into something called disability-adjusted life years (DALYs: in essence, you ‘gain’ DALYs for dying soon or being sick, so fewer is better. So, how many DALYs does a doctor save?
- A five-year life expectancy increase is easy: five more years of life, so five DALYs averted.
- ‘Five years relieved from poorer health’ is trickier. How bad is life with different sorts of ill health — and how this compares to life in good health (e.g. would you rather live x years longer in good health or x+n years with heart failure?) — remain fraught questions.10 Playing very fast and loose, let’s give the ‘poorer health’ being relieved a disability weighting of 0.2511, so relieving this is ‘worth’ 5 x 0.25 = 1.25 DALYs averted.
- So the average ‘DALY per person’ effect is living five years longer (5) + 5 years without 0.25 disability (5 x 0.25 = 1.25). Combining the two gives 6.25 DALYs averted by medical care.
- Let’s now allocate all of this benefit to doctors for now. The UK has ~3 doctors per 1,000 people. So — again, roughly — we can take the population level impact (6.25 x 1,000 = 6,250 DALYs), then divide by the number of doctors (3) to get the impact of a UK doctor over their career: 6,250/3 ~ 2,100 DALYs averted.
‘How many DALYs does a doctor save?’ is not exactly ‘How many lives does a doctor save?’ There’s a facetious answer to the latter question: none, as everyone dies eventually. Perhaps a better one is taking a ‘life saved’ as (very roughly) equivalent to 30 DALYs: if you stop me dying now but I die in my 60s, this seems the sort of impact we have in mind with ‘saving a life’ (contrast this with, for instance, forestalling my death at 85, but I die two years later).
So 2,100 DALYs averted divided by 30 comes to 70 ‘lives saved.’ Assuming a 40-year or so medical career, the typical doctor saves a couple of lives each year. This is pretty good — even if other careers might be better on this metric.
However, this figure is not only a rough estimate, but an overestimate. One key reason is that it overestimates by neglecting to account for diminishing marginal returns, which we turn to in Part 2.
Read next: How many lives does a doctor save? (Part 2)
To further refine our estimates of how many lives a doctor can save, we must account for diminishing marginal returns.
Learn more:
- Read our in-depth career guide
- Problem profile: Preventing catastrophic pandemics
- Career review: Biorisk research, strategy, and policy
- Podcast episode: Dr Pardis Sabeti on the Sentinel system for detecting and stopping pandemics
- Podcast episode: Elie Hassenfeld on two big picture critiques of GiveWell’s approach, and six lessons from their recent work
- Podcast episode: Andy Weber on rendering bioweapons obsolete and ending the new nuclear arms race
Notes and references
- This article focuses on the UK. But as we’ll see, the UK story generalises well to other high-income countries.↩
- From the Global Burden of Disease 2019 paper:
 ↩
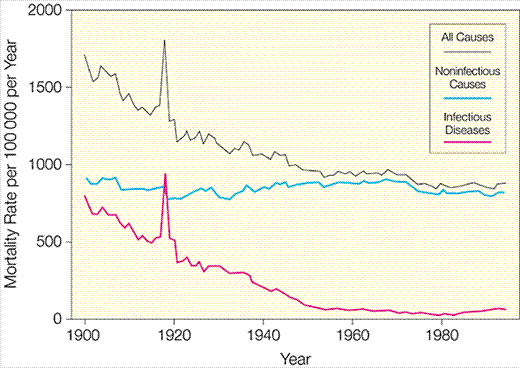
↩ - See McKeown, T (1976) The role of medicine: Dream Mirage or Nemesis? (p 81). For reassurance this canonical example is not a cherry-picked outlier, see (e.g.) this paper of US infectious disease mortality:

We again see a large secular decline in infectious disease mortality (note the very large aberration due to the 1918 influenza pandemic, and a reversal in trend from 1980 likely owed to the AIDS pandemic), in which a lot of the decline happened before effective medical countermeasures were developed. Penicillin was discovered in 1928, by which time US infectious disease mortality had already dropped by half. Although some vaccines were discovered earlier than this (and smallpox variolation was widely used in the US prior to 1900), most of the routine vaccines — starting with Polio — were discovered and deployed from the 1950s onwards; by 1950, infectious disease mortality had fallen by ~90% from 1900.↩
- The common challenge is that populations in poorer places and times tend not to carefully record data on their experience of disease, death, and deprivation. Although high-quality birth and death data can extend into the 19th century, for many other measures (e.g. death by cause, disaggregated economic activity, primary school completion rate, etc.) ‘records began’ somewhere between 1900 and 1950, and you have to wait until 1990 to get global coverage good enough for efforts like the Global Burden of Disease project. Numbers before then tend to be mixes of rough estimates and expert speculation.
I still think this gives good support for the social determinants story of disease, even if large parts of it are hypothesised to have happened before data was recorded: whenever you happen to start recording, you see steep declines happening as soon as you start measuring it. A broad decline in ill health which is picked up at various points along the way by the data seems the best explanation.↩
- The two index studies for ‘RCTs’ on healthcare provision’ are the Oregon Medicaid health experiment and the RAND Health Insurance Experiment. The treatment group with cheaper/free access to healthcare generally had marginal improvements in measures of health: in the Oregon study, although measures like blood pressure and cholesterol favoured treatment, none reached statistical significance; in the RAND study there is a signal for those at highest risk given free care, but other indicators (whether for subgroups or not) were mostly flat.
This data could be argued either way: despite sample sizes in the tens of thousands, these studies would be underpowered for any particular condition (save blood pressure, where most of the significant results are found), so perhaps these studies are still underpowered to detect many of the health benefits of healthcare. But free or discounted healthcare gave the treatment a significant benefit in-kind: for poorer households, the benefit was worth between one-third to two-thirds of their household income — perhaps they would have ended up even healthier if they were given the face value of the insurance in cash instead.
Still — and notwithstanding how far these US results should be generalised — it seems fair to say these weigh against the conclusion that healthcare has a dramatic impact on health.↩
- See, for instance, “The Contribution of Medical Care to Mortality Decline:
McKeown Revisited” by Johan P. Mackenbach.↩ - This sometimes goes under the charming phrase “competing causes of death.”↩
- We have mostly glossed over issues of quality as well as length of life. A common worry is the “expansion of morbidity”: although we are saving (really, extending) lives, this added lifespan is one with lots of ill health and disability. A morbid old age is a fate better than death, but less than we might hope for.
The GBD uses DALYS, composed of years of life lost and years lived with a disability: both components are in steady global decline. In terms of ‘healthy’ or ‘disability-free’ life expectancy, these have increased roughly in proportion to life expectancy gains (both worldwide and for wealthy countries like the UK). So, although years lived in ill health have increased in absolute terms, one can expect to live a similar proportion of one’s life free of disability than in 1990. Although data is scarce and interpretation tricky, I think the picture is one of qualified reassurance.↩
- They are also likely overestimates. First, the additional life expectancy credited to medical interventions are unlikely to be at full health. Second, the technique for the estimate uses clinical trial data, and trials typically overestimate ‘real world’ performance of interventions when used in routine practice.↩
- DALYs (and similar metrics) are principally a tool for health economics to compare interventions between diseases: all else equal, a treatment that mildly improves dementia may be better than a complete cure for knee arthritis, because dementia could be much more important to someone’s overall health. DALYs let you quantify these differences with numerical disability weights (from 0 = full health, 1 = no better than death), and so prioritise health spending. So — for example — (moderate) knee (osteo)arthritis gets 0.079; (moderate) dementia 0.377. These also give trade-offs between length and quality of life: so ~ 12 years without mild osteoarthritis is as good as 1 extra year of healthy life; for dementia it is ~3.
Such numbers abbreviate many controversies:
- It is unclear what these weights should — or should not — be capturing: subjective well-being? Economic productivity? Impact on relatives/carers? A poll on a population’s preferences?
- It is also unclear what these weights in fact capture: typically, those with a given condition rate it as less severe than the general public (cf.).
- Application is often controversial: DALYs and similar measures can imply those with permanent disabilities should be deprioritised for medical care versus those without them (e.g. if I have dementia and you do not, extending your life by five years is ‘worth’ 5 DALYs, but extending mine by the same is only worth ~3 DALYs).
I can’t answer these problems in a footnote — not least because I don’t know the answers myself. Fortunately, for our purposes, DALYs do not need to be perfect, but only good enough for a rough estimate to capture ‘quality of life’ improvements. Given social determinants are more ‘preventative’ than ‘disease modifying,’ rejecting such measures and only looking at lifespan and mortality would further discount the impact of medicine.↩
- Any number between 0.1 and 0.5 is defensible. I got to 0.25 by comparing the conditions Bunker highlights as ‘medical intervention success stories’ and eyeballing their (untreated) disability weights here.↩